Support for Avoidant Restrictive Food Intake Disorder (ARFID)
These pages have been created by the North East and North Cumbria (NENC) Provider Collaborative. They are for the benefit of all those living with ARFID/suspected ARFID and their carers across the region. Resources on this website have been co-produced with experts from other national services, and with those with lived experience.
-
What is ARFID?
Avoidant restrictive food intake disorder (ARFID) is a diagnosable eating disorder. It is characterised by avoiding certain foods or food groups and/or restricting the amount of food eaten.
The reasons why someone may be restricting and/or avoiding their food intake varies between individuals. However, they are usually associated to one or more of the following:
- Sensory-based food avoidance. This means having a very sensitive dislike to the sensory properties of food. This includes the taste, appearance, texture, temperature or smell of certain foods or food types.
- A phobia or fear of the aversive consequences of eating. Such as a food-associated fear of vomiting, choking or contamination. This may have come from a negative experience (trauma) that is experienced or witnessed. Examples of traumatic experience can include a sickness bug or choking episode.
- Poor recognition of hunger or a poor appetite, resulting in a very low interest in eating.
You can see from this diagram that there is often more than one reason behind the food avoidance and restriction:
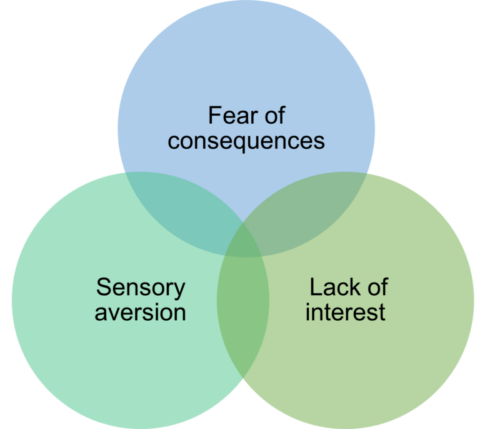
Although the reasons can be different, all people who develop ARFID share the same characteristic. They all avoid or restrict their food intake by reducing the overall amount eaten, by limiting the range of foods eaten, or both.
ARFID cannot be due to lack of available food or due to cultural norms. For example, you cannot be diagnosed with ARFID if you are fasting or choose not to eat certain foods for religious or cultural reasons.
ARFID is also different to other restrictive eating disorders in that:
- A person with ARFID isn’t affected by their beliefs about the size and shape of their body
- A person with ARFID doesn’t restrict their food intake to intentionally lose weight
If you (or your loved one) are restricting your food intake due to concerns about weight, shape or body image you may need different support. If you suspect that you (or they) may be suffering from another eating disorder please contact your local GP. Other eating disorders include disorders like Anorexia Nervosa and Bulimia Nervosa. Your GP will be able to offer advice, guidance and signposting to the right support in your local area. -
What is ARFID? (a lived experience perspective)
This poem was written by Shelley Murray-Foreman (2022). It was written for her young son to help raise awareness ARFID. She also wanted it to improve the understanding of living with the condition:
Hi! My name is Joseph-Jason
But you can call me Dude
And I am here to explain to you
How I feel about drink and food.I have this thing called ARFID
But it doesn’t make me weird
I just find most food scary
It’s something to be feared.My Mummum calls me Scrawny Butt
Because I am so thin
But it’s not like anorexia
I can’t control it I don’t win.Some people just don’t understand
“If he’s hungry he will eat”
“Don’t give in to pickyness”
“If you don’t eat, no treat”But I would rather starve myself
Than risk a taste or lick
I won’t eat food I don’t deem safe
This is real: it’s not a trick.Don’t slip things in my safe food
Because I’ll know, then that’s gone too
And then do you know what happens?
I’ll never trust food from you!My safe foods are brand specific
‘New and inproved’ is my worst nightmare
If the packaging or product changes
I can’t eat it and that’s not fair.So when you see us eating
My family has a proper meal
Please don’t make rude comments
Don’t make it a big deal.If, like Shelley, you would like to share any of your own experiences please email the ARFID project lead [email protected] – we’d love to hear from you!
-
I don’t have a diagnosis of ARFID. Is this information for me?
It is important to note that not all people with symptoms of avoidant eating have an ARFID diagnosis. This may be because they have concerning restricted eating which wouldn’t meet the ARFID diagnostic criteria. This is known as extreme selective eating. Or it may be because no formal assessment has taken place.
All the content on our website provides reliable and helpful information. Reading support books, websites, self help guides and webinars for ARFID are all examples. They can all help to provide you with knowledge and strategies to approach food and eating change. You don’t need a diagnosis to use these. You just need a sense that these strategies are a good fit for the symptoms that you, or your child, is experiencing.
-
How do I know if it’s ARFID or 'fussy eating'?
It is normal for all children to go through a ‘fussy’ or selective eating stage during their development. It is also normal for children to have periods of a very high appetite which move into periods of eating very little. This change in eating is usually due to their current growth patterns, levels of activity or whether there has been a period of illness. Fluctuations in the amount of food eaten from day to day are not a concern for children where they are healthy and continuing to grow.
Adults can also have more selective eating preferences. They could choose to eat the same meal/meals daily, choose from a limited selection and have preferred brands that they like. Adults can also prefer to eat at certain times, in certain places or in a planned way. Just like adults who eat a wide variety of foods, spontaneously and in different places – these are all examples along a spectrum of ‘normal’. Food selectivity becomes a problem when the type or amount of food impacts your weight or physical health because you do not eat enough energy, protein and/or vitamins and minerals. It also becomes a problem if it impacts your ability to enjoy your usual social activities, go to work/study, worsens your mental health and wellbeing.
To read more about the difference between ARFID and Picky eating please see this blog post:
Eating is actually quite a complex process – Dietitians Sarah Fuller and Clare Ellison on ARFID vs ‘picky eating’This article has been co-written by the North East and North Cumbria ARFID Project lead with BEAT, the national eating disorders charity.
If you are a carer, you can also use this helpful ‘picky eating screener’ tool to help you think through whether your child has picky eating or you should be more concerned. It comes from an expert dietitian-led website in America and can be a useful and practical first step: Picky Eating Screener – Kids Eat in Color
Our colleagues at the Hywel Dda Health Board in Wales have also created this excellent restrictive eating self assessment resource to explore concerns around the degree of selective eating patterns.
-
What are the problems associated to having ARFID?
Due to the significant restriction of intake, those living with ARFID may experience*:
- Weight loss
- Growth delays (in children)
- Hormonal changes (including a loss of periods in girls and women)
- Nutritional deficiencies resulting in a range of physical health impacts
- Reliance on daily micronutrient support or nutritional supplements
* this is not an exhaustive list
Both those with ARFID, and their carers, can experience:- Social isolation from feeling unable to partake in social or family activities/events, school/work or take holidays
- Low mood
- Anxiety associated to the impacts of ARFID. This includes worrying about eating with others, needing fixed meal times and/or types of foods and intense worry if these plans change
- Financial pressure from needing to buy specific or branded food items, or from food waste
- Health worries for themselves or their loved one
-
Understanding more about ARFID
If you’d like to understand more about ARFID you can view our co-produced NHS-England film featuring both clinicians and a parent story here: NHS England ARFID Awareness Film (youtube.com)
The film’s ARFID awareness leaflets can also be found here:
ARFID Parent Carer leaflet
Easy Read ARFID Parent Carer leaflet -
Debunking the myths about ARFID
Myth: ARFID only affects children
ARFID is frequently believed to only impact children and adolescents. The idea of being a “picky eater’’ (selective eater) is often associated with children. This can make it difficult to recognise and validate adults who suffer with ARFID. Although ARFID is more common, with more research done in children, it is not a childhood illness. ARFID can begin in childhood and continue into adulthood. A person can also transition from selective eating to ARFID at any age or developmental level. Lastly, ARFID can start at any age due to different triggers (such as trauma).Myth: You have to be underweight to have ARFID
It is often assumed that if you restrict your intake, you must be underweight. However, ARFID is not an exclusively low weight eating disorder. This means that for some, weight and growth will be impacted. This is because there is a restriction in the over-all energy eaten. But for others, they may be normal or over-weight. This is due to their limited range of foods containing a large amount of calories (energy). A person with ARFID can be malnourished, with micronutrient deficiencies, and yet ‘look’ well nourished. It is important that for those with ARFID, a judgement about severity or risk is not based only on weight.Myth: ARFID is just ‘picky eating’
ARFID is recognised as a mental health disorder in the manuals we use for diagnosing psychiatric difficulties (DSM-5 and IDC-11). There is more to ARFID than ‘picky eating’. Selective eating is often a phase and does not produce any significant long-term consequences. With ARFID, a person avoids food to the point that their physical and psycho-social health is compromised. This is much more disruptive to a person’s life than selective eating is.Myth: ARFID doesn’t cause serious health issues
ARFID can lead to severe consequences, including weight loss, nutritional deficiencies, growth delays in children, or an increased risk of medical complications like scurvy, osteoporosis and anaemia.Myth: It’s the parents’ fault
Parents do not cause ARFID. Caring for a young person with ARFID is very difficult and challenging and it is not their fault. It is true to say that there are ways of approaching the challenges of ARFID which can be more, or less, helpful. But the most important message is that the support of families is part of the solution – not part of the problem.Myth: It’s a choice – they’re just being difficult
Living with ARFID is very difficult. It negatively impacts your mental health, reduces your social opportunities, and significantly impacts your physical health. People living with ARFID are not choosing to live this way, they are not being difficult and they are not to blame.Myth: Everyone with ARFID is autistic
Autistic people often have more sensory sensitivities. This means that ARFID is more common in autistic individuals. However, you can have ARFID without being autistic and you can be autistic without having ARFID. -
Tips and advice
Here you will find our ‘Simple Suggestions Series’: a range of resources for parents/carers, schools, adults or advice across the ages. These resources have been co-developed by:
- Clare Ellison, Advanced Eating Disorders Dietitian and ARFID Project Lead, Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust
- Paola Falcoski, Advanced Eating Disorders and ARFID Dietitian, with certificate training in autism, East London NHS Foundation Trust
- Ursula Philpot, Consultant Dietitian and Clinical Associate for North East and Yorkshire Regional Mental Health Team, InsightEating
All our SSS resources include input from parents/carers and patients with lived experience of ARFIDFor your child
How can schools support a child with ARFID?
Creating supportive mealtimes
Helping your child add new foodsFor adults
Changing your eating environment
Strategies to support you in challenging a fear (aversive consequences)
Strategies to aid you in adding new foods
Creating your own ideal supportive mealtimeFor all ages
Strategies for planning and managing a holiday away from homeOur colleagues from the Aneurin Bevan University Health Board (Wales) have also created this excellent patient resource for parents and carers of children who have a fear of swallowing.
This patient resource about how to achieve ‘5-a-day a different way’ has been co-produced by British Dietetic Association ARFID group and the British Dietetic Association Learning Disabilities group. It is suitable for all ages.
We have also developed a practical tools and advice resource for patients (or their families) admitted to a hospital ward for treatment for their sensory restrictive eating disorder. This is when a person restricts their eating because of the sensory properties of the food and/or environment. These individuals would usually need adaptations for their sensory differences to support an effective admission.
-
Psychoeducation Webinar series for parents and carers
This video webinar series aims to provide accessible information on a range of topics for parents and carers of children with ARFID. The series has 8 ‘modules’ and each module is broken down into smaller bite-size videos. You can choose to watch all the modules in sequence, or simply pick the topics that are most interesting and relevant to you. It also gives you the freedom to return to any topics as often as you need. All videos include subtitles.
We understand that long resources, books, websites, and workshops can sometimes feel too much with so much else going on. So, if you need information quickly and easily – this small series is created for busy parents with little spare time!
To access subtitles on these recordings, please turn these on using the YouTube video functions.
Module 1 – What is ARFID?
Signs and symptoms of ARFID
Early vs late onset ARFID
General treatment approaches
What ARFID isn’tModule 2 – Understanding ARFID more
Neurodiversity in ARFID
Understanding safety behaviours in ARFID
How does a limited diet maintain ARFID?
Understanding hunger and fullness
Recovery limiting behaviours
ARFID can lead to other eating disordersModule 3 – Supporting a helpful environment
The occupational therapy role
Physical and environmental factors
The food environment
The meal time environment
Routines and timetables
Mealtimes for children with autism
Co-regulation and reducing negative associationsModule 4 – Understanding the role of the senses
Mealtimes as a sensory experience
Understanding interoception
The senses
Over responsivity and under responsivity
Messy playModule 5 – Nutritional assessment and recovery
Growth, development and weight in ARFID
Nutrient deficiencies and supplements
Risks and treatment targets in ARFID
When you may need to see a dieticianModule 6 – Communication skills and parenting style
The family are not to blame
Helpful and less helpful things to do
Additional tips for very young children
Starting a conversation with your child
Parental expectations of change
Managing anxietyModule 7 – Options for approaching change
Finding the right approach
Making goals
What is CBT?
Understanding food chainingModule 8 – Getting help
Starting a conversation with schools and services
Supporting your own mental health
What do I do if it’s not working?Content created by:
 Clare Ellison, Advanced Eating Disorders Dietitian, ARFID Project Lead for the North East and North Cumbria Provider Collaborative, BEAT Dietetic Clinical Advisor and British Dietetic Association ARFID Committee Member. Clare has extensive clinical eating disorder experience in working with adults, and children and young people and their families. Clare has also developed ARFID clinical practice guidelines, extensive resources, and delivers training and supervision.
Clare Ellison, Advanced Eating Disorders Dietitian, ARFID Project Lead for the North East and North Cumbria Provider Collaborative, BEAT Dietetic Clinical Advisor and British Dietetic Association ARFID Committee Member. Clare has extensive clinical eating disorder experience in working with adults, and children and young people and their families. Clare has also developed ARFID clinical practice guidelines, extensive resources, and delivers training and supervision.  Ursula Philpot, Consultant Eating Disorders Dietitian at InsightEating, Clinical Associate with the North East and Yorkshire Regional Mental Health Team, Senior Lecturer with Leeds Beckett University and British Dietetic Association ARFID Committee Member. Ursula has extensive clinical experience in working with children and adults with eating disorders, including ARFID. She has also delivered regional ARFID staff training, worked on ARFID developments nationally with NHS-England, has developed an ARFID clinical Champions programme and provides supervision.
Ursula Philpot, Consultant Eating Disorders Dietitian at InsightEating, Clinical Associate with the North East and Yorkshire Regional Mental Health Team, Senior Lecturer with Leeds Beckett University and British Dietetic Association ARFID Committee Member. Ursula has extensive clinical experience in working with children and adults with eating disorders, including ARFID. She has also delivered regional ARFID staff training, worked on ARFID developments nationally with NHS-England, has developed an ARFID clinical Champions programme and provides supervision.  Tara Tordoff, Advanced Paediatric Occupational Therapist at the Great North Children’s Hospital (Newcastle Upon Tyne Hospitals NHS Foundation Trust). Tara has worked in both hospital and community settings and was involved in delivering training for the ‘Sensational Thinking Project’. This delivered education to families, schools and professionals involved in the care of children with sensory processing differences. Tara is very passionate about helping families to support and identify difficulties within feeding and food handling, such as in those with ARFID.
Tara Tordoff, Advanced Paediatric Occupational Therapist at the Great North Children’s Hospital (Newcastle Upon Tyne Hospitals NHS Foundation Trust). Tara has worked in both hospital and community settings and was involved in delivering training for the ‘Sensational Thinking Project’. This delivered education to families, schools and professionals involved in the care of children with sensory processing differences. Tara is very passionate about helping families to support and identify difficulties within feeding and food handling, such as in those with ARFID. Nicole McCook, Specialist Paediatric Occupational Therapist at the Great North Children’s Hospital (Newcastle Upon Tyne Hospitals NHS Foundation Trust). Nicole has worked in both hospital and community settings and has recently co-established food play groups. Nicole is currently working on a child development project on preparation for feeding. She is interested and very passionate about helping families to support and identify difficulties within feeding and food handling, such as in those with ARFID.
Nicole McCook, Specialist Paediatric Occupational Therapist at the Great North Children’s Hospital (Newcastle Upon Tyne Hospitals NHS Foundation Trust). Nicole has worked in both hospital and community settings and has recently co-established food play groups. Nicole is currently working on a child development project on preparation for feeding. She is interested and very passionate about helping families to support and identify difficulties within feeding and food handling, such as in those with ARFID. Dr Hannah Harvey, Highly Specialist Clinical Psychologist with Durham and Darlington Children’s Eating Disorders Team. Hannah has extensive clinical experience working with Children with mental health difficulties and eating disorders services. She has also worked with the children and young people’s autism assessment team. Hannah is highly skilled at adapting psychological interventions for young people with Autism and has ARFID service development experience.
Dr Hannah Harvey, Highly Specialist Clinical Psychologist with Durham and Darlington Children’s Eating Disorders Team. Hannah has extensive clinical experience working with Children with mental health difficulties and eating disorders services. She has also worked with the children and young people’s autism assessment team. Hannah is highly skilled at adapting psychological interventions for young people with Autism and has ARFID service development experience. -
Common ARFID Questions and Answers (Q&A) with a multi-professional panel
The North East and Yorkshire Regional Mental Health Team hosted three public Q&A panel events in 2024. These three sessions gave parents and carers of those caring for a young person with ARFID the opportunity to ask questions to a panel of different care professionals. The panel included an expert dietitian, psychologist and occupational therapist.
The public pre-submitted questions before the event and there were over 100 questions submitted per one hour session. Therefore, to be as helpful as possible, these questions were grouped together into ‘question themes’. The panel then answered these question themes with some limited time to answer questions asked on the day. Sessions were recorded and the events can be watched again here:
ARFID parent/carer Q&A 1-2pm
ARFID parent/carer Q&A 6-7pm
ARFID parent/carer Q&A 5.45-7pmThere were several resources for further support that were mentioned during these events. All these resources can be found under the different headings on this website.
The events were evaluated, and the NEY-Regional Mental Health Team are currently considering how future events could be run.
-
Where can I find more information and self-help material?
The ARFID Awareness UK website includes information and resources. The site shop also includes options to purchase cards which help inform schools and restaurants about the disorder.
For carers of children with ARFID, arfidkids.com is a wonderful, comprehensive resource.
Longer webinar videos for parents/carers are available to watch from Aneurin Bevan University Health Board (Wales). They present slides with talking but without subtitles. Available from the Aneurin Bevan University Health Board website
A range of books is also available including:
- ARFID Avoidant Restrictive Food Intake Disorder: A guide for parents and carers by Rachel Bryant-Waugh
- Helping your child with extreme picky eating by Katja Rowell & Jenny McGlothlin
- The picky eater’s recovery book by Jennifer Thomas
Can’t eat, won’t eat by Brenda Legge
This Instagram account helps to understand support through food chaining: @feedingpickyeatersSelf Help Material
South Yorkshire Eating Disorder Association website (SYEDA) has an ARFID self-help course for individuals (adults) struggling with the symptoms of ARFID. You can move through the 4-step programme at your own pace. The 4 modules include:- Learning about ARFID and making some early changes
- Continuing early changes and setting big goals
- Facing your fears
- Preventing relapse
Written self-help material for young people or their parents/carers is available in the modules from the Be Body Positive website. These include information as well as practical suggestions to support your journey.For teenagers with co-occurring autism, The Autistic Teens Avoidant Eating Workbook by Elizabeth Shea is available to buy. This is a guide designed to help you recognise the signs of avoidant eating, cope with food related anxieties and manage sensory overload. It also supports through the particular social stresses of communal eating. The book includes top tips, a progress tracker, quizzes and worksheets.
-
Is there any information specific to younger children?
The Sensory Oral Sequential, known as the SOS approach to feeding offers a two hour parent education seminar. It is delivered by expert Dr Kay Toomey who leads on SOS feeding and is available on the SOS website.
Additionally, this toolkit is a fun free way to help avoidant, picky, and fussy eaters: www.sensoryplaytoolkit.weebly.com
-
Are there any forums to support me with my ARFID symptoms?
The national eating disorders charity BEAT offers a confidential and inclusive space for anyone who has, or thinks they might have, ARFID. The Hummingbird Online Support Group currently runs on Sundays 6.45pm-7.45pm. Find out more on the BEAT website where you can also find Peer support and online development for carers (POD sessions) and further information on Support for Carers
ARFID Awareness UK also offers online virtual community support options for individuals or carers.
-
Are there any local face-to-face ARFID carers support groups available?
A free in-person ARFID carers support Group is available in Teeside. The sessions are held monthly at Make Believe, Cromwell Street, Hartlepool TS24 7LR. For more information on the sessions please contact Katie Jones on 07504 420 412 or email [email protected]
You do not need to be from Teeside to attend. There is also a Teesside ARFID parent/carer facebook group
Owl Blue is a registered charity based in West Cumbria that provides free support to individuals and families affected by, or suspected of having, neurodivergent conditions. The organisation hosts a free ARFID support group monthly, called “Owl Blue ARFID Friends Support” which is held locally in Maryport, and if interested, individuals can access the organisation’s private Facebook page or they can contact Owl Blue on 0800 755 5432 or [email protected]
Eating Distress North East (EDNE) is a charity based in the North East offering a variety of support options for those with Eating Distress, including ARFID:
- Counselling – EDNE offers free 1 to 1 confidential counselling sessions to people with eating distress who live anywhere in the North East of England aged 16+. This includes people with an ARFID type presentation. You do not need to have a medical diagnosis of an eating disorder to access this service. Counselling sessions can take place in person at our offices in Newcastle, outreach bases at Chester-le-Street, Stockton, Hartlepool, or online via Teams. All counsellors are fully qualified; registered with the British Association for Counselling and Psychotherapy (BACP), UK Council for Psychotherapy (UKCP) or equivalent; and are either accredited or working towards accreditation. They are also experienced in working with people who have eating distress and disorders, and undertake regular continual professional development in specialisms including: working with neurodivergent clients; working with LGBTQ+ clients; gender issues; children and young people; working with family members; anticipatory grief and bereavement, and more. To access this service please register with us.
- Groups – EDNE offer online one-off topic groups. Topics include anxiety, self-care, sleep, emotions, and interoception. We have 4- and 5-week specific groups which are held at our office in Newcastle. Themes are ADHD and eating distress, Body Image, and ARFID. You can refer via our website and if you only wish to access groups, choose “groups” as the service you are interested in. To access this service please register with us. People in counselling with EDNE can also access groups with us after an initial assessment.
- Parents/carers – EDNE can offer a one-off counselling session with one of their qualified counsellors. You might find it useful as a space to share your worries, frustration, or hopelessness you are feeling in the caring/supporting role. You might want to specifically ask questions about the eating distress/disorder your loved one is experiencing to increase your knowledge. To register for a one-off counselling session, please complete the registration form and choose the “one-off counselling session” option.
-
Are there any forums to support me as a carer?
Caring for a loved one with ARFID can feel overwhelming, restrictive and worrying. It is very important to take care of your own mental wellbeing and seek support where this is helpful to you.
Available peer support options for this include:
Peer support and online development for carers (POD sessions) are available via the national eating disorders charity BEAT. There, you will also find further information on Support for Carers – This includes links to wider charities such as those for financial guidance. It also includes many sources of support for your own carer wellbeing.
ARFID Awareness UK offers online virtual community support options for carers.
ARFID UK for professionals and parents is a Facebook Group support option
-
Where can I find more information on sensory difficulties?
The Humber Sensory Processing service have helpful resources on interoception strategies as well as more generic information on sensory processing and sensory learning
The National Autistic Society also host information on sensory differences for all audiences
Locala offer practical sensory toolkits for use with schools, young people and families.
-
My child struggles to take medication or vitamin and mineral supplements. Is there any advice?
This helpful blog offers advice and information to support support autistic children and young people with taking medications. This advice is also applicable to those with sensory differences, and can be used for supporting taking vitamins and mineral variations too: Sensory overload: Teaching children with autism to take medication
-
Where can I find more information and support for autism?
The National Autistic Society has a guide for all audiences on eating problems
Further information on supporting autistic people with eating difficulties is also available.
Dr. Pooky Knightsmith is a prominent keynote speaker, author and advisor. Her work uses her education and lived experience of autism, eating disorders and mental health struggles. She offers practical ideas, information and education. Her YouTube channel covers a range of associated neurodiversity challenges. Alternatively, you can also visit her website
Extensive information and support is also available for patients and carers from: www.peacepathway.org/ This includes information on supporting and creating helpful meal environments
One example of a helpful book is Food refusal and avoidant eating in children, including those with autistic spectrum conditions: a practical guide for parents and professionals by Gillian Harris (available to buy in print).
This selective eating affirmations resource – AutisticMeltdowns – can also be helpful. This is particularly true for those individuals who do not have ARFID, but do have a limited and more selective intake.
It comes from the Lived Experience Educator website which hosts a lot of valuable content for neurodivergent individuals.
-
Is there any support for Pathological Demand Avoidance (PDA)?
PDA is typically understood as Pathological Demand Avoidance. However, recent thinking is reshaping this term to instead understand it as being a Persistent Demand for Autonomy.
Persistent Demand for Autonomy is a strength-based language which is experienced as much less blaming and shaming. At NENC we prefer to use this terminology and prefer to seek a ‘strength based’ understanding. However, we recognise that most published literature and support refers to demand avoidance. This is therefore what is described below. But we would encourage you to re-frame your own understanding of these challenges to meaning a persistent demand for autonomy, instead.
‘Demand avoidance’ involves not being able to do certain things at certain times. This is a normal human trait. Avoiding demand is something we all do to varying amounts and for different reasons. This means it is on a spectrum. More significant demand avoidance can be due to a wide variety of reasons.
Autistic people may more often avoid demands that trigger anxiety or sensory overload, or which disrupt routines. These demands may cause them to refuse, withdraw, ‘shutdown’ or escape to avoid these things.
Pathological demand avoidance is all-encompassing. It has some unique aspects including avoiding everyday demands simply because they are demands.
If you feel that you, or a loved one, may be struggling with demand avoidance or you wish to find our more, the following pages offer further information:
PDA Society – Pathological Demand Avoidance
National Autistic Society – Demand avoidance -
Is there any support for PICA?
Pica is an eating disorder in which a person eats non-food substances with no nutritional value. For a diagnosis of pica, the behaviour must be present for at least one month, not part of a cultural practice, and developmentally inappropriate. This means that it is generally diagnosed in those younger than 2 years old. Pica affects people of all genders and ages, though it is more likely to first appear among children. People with pica don’t usually avoid regular food, meaning they may still be getting all the nutrients they need. However, some non-food items that they consume can be very dangerous, especially if eaten in large quantities.
The IDiscover team at Northamptonshire Healthcare have produced an excellent parent and carer guide for Pica though please note that because this is not a NENC resource, the information about service signposting (page 15 and 16) is not applicable to our local residents. Please see your GP or health visitor for further advice and signposting.
Useful links for further support include:
-
It’s not working! Where do I go?
Sometimes, despite your very best efforts you may find that the restrictive eating is worsening.
If you are concerned about the health, growth and development of yourself, or your child, please visit your local GP (or health visitor). They will be able to offer advice and signposting to the appropriate local service(s) in your area.
If there is a sudden and rapid restriction in food or fluids that has led to sudden deterioration in physical health please seek help quickly. This may include contacting NHS-111 or emergency care services. Sudden deterioration is often a result of a traumatic event leading to a rapid avoidance of food and/or fluids.
If there is a sudden deterioration in mental health, or you are concerned about mental health risks, please contact your local crisis or emergency care services. Mental health risks include, but are not exclusive to, suicide and self harm.
If you wish to contact a helpline you can do so via the BEAT Helpline on: 0808 801 0677 Available Monday-Friday 9am-8pm, and weekends 4-8pm.
Please note that this is not an emergency care service.
-
Get involved
Lived experience is at the heart of everything we do. It has been included in, and shaped, all that we have created and shared as part of the ARFID project. If you, or your loved one, would like to help influence our ongoing work and get involved we’d love to hear from you. Please get in touch with our project lead by emailing [email protected]
-
Website validity information
This website was reviewed by Clare Ellison (ARFID Project Lead) in February 2025.
Updates are added as relevant and appropriate, however the full content of the website is next due for comprehensive review in February 2026.
